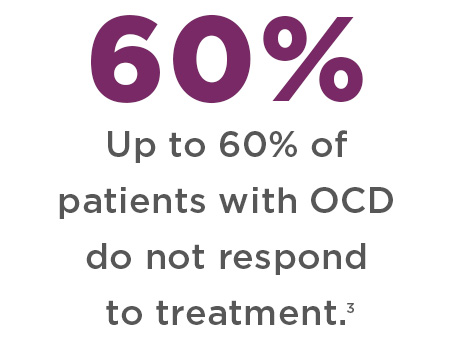
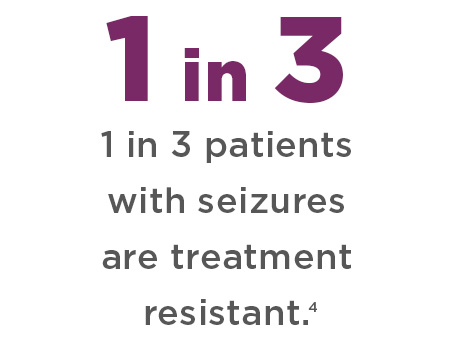
Still struggling with treatment-resistant symptoms?
An autoimmune response could be causing your neuropsychiatric symptoms.
An autoimmune response could be causing your neuropsychiatric symptoms.
In some individuals, common infections (i.e. strep, influenza, mycoplasma, Epstein Barr virus and Lyme disease) can trigger an abnormal immune response. Antibodies produced to destroy a harmful pathogen (i.e., bacteria, virus), mistakenly attack healthy cells in the brain. This autoimmune response can disrupt how neuronal cells function and cause inflammation in the brain, leading to various neurologic and/or psychiatric symptoms.
One study found the risk of developing a psychiatric illness was increased further depending upon the number and severity of infections the individual had. 1 And researchers suggest, “a wide variety of infections, even common ones like bronchitis, are linked to a higher risk of many mental illnesses in children and adolescents.” 1
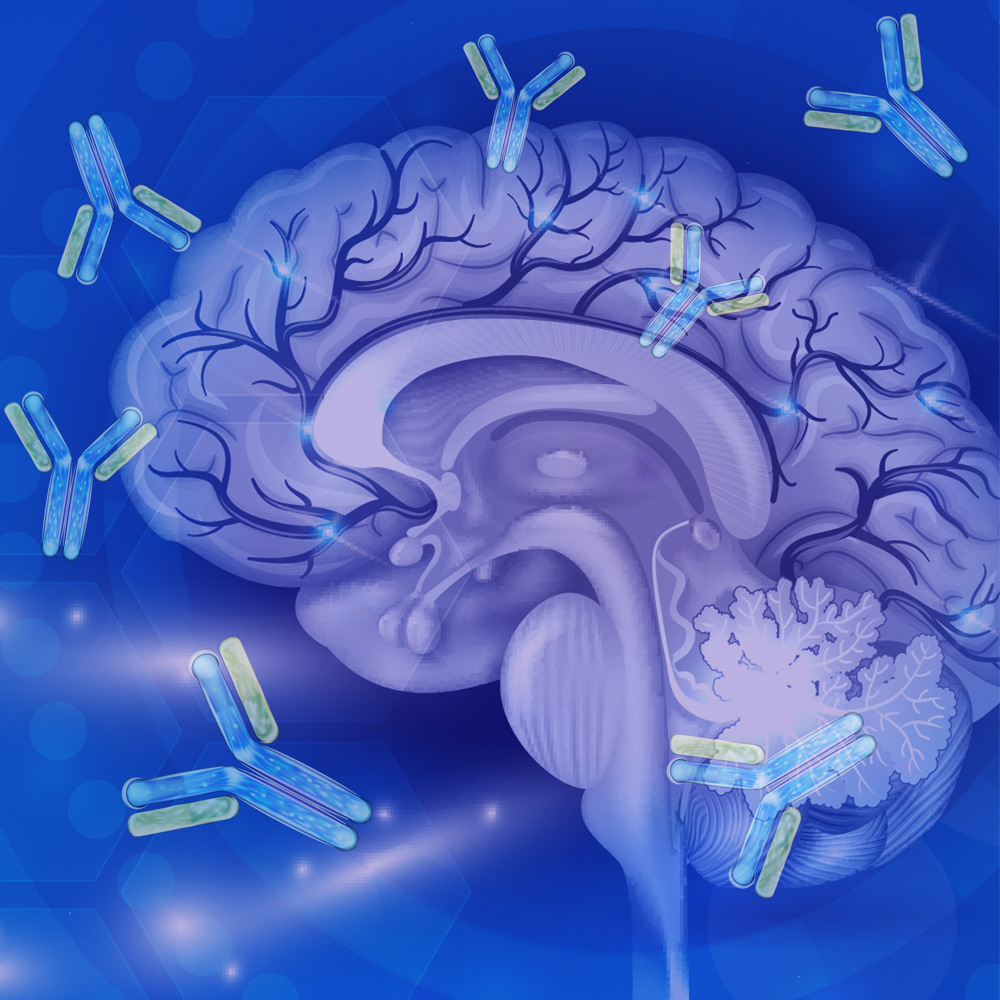
The brain used to be considered immune privileged and protected by a “blood-brain barrier.” That is, antibodies produced by the immune system could not enter the brain. But we now know that infections and inflammation can open up the blood-brain barrier, permitting these autoantibodies to enter the brain and trigger central nervous system disorders, including neuropsychiatric conditions. 2
In some cases, treatment-resistant neuropsychiatric symptoms may be due to an infection-induced autoimmune response.
You get
an infection
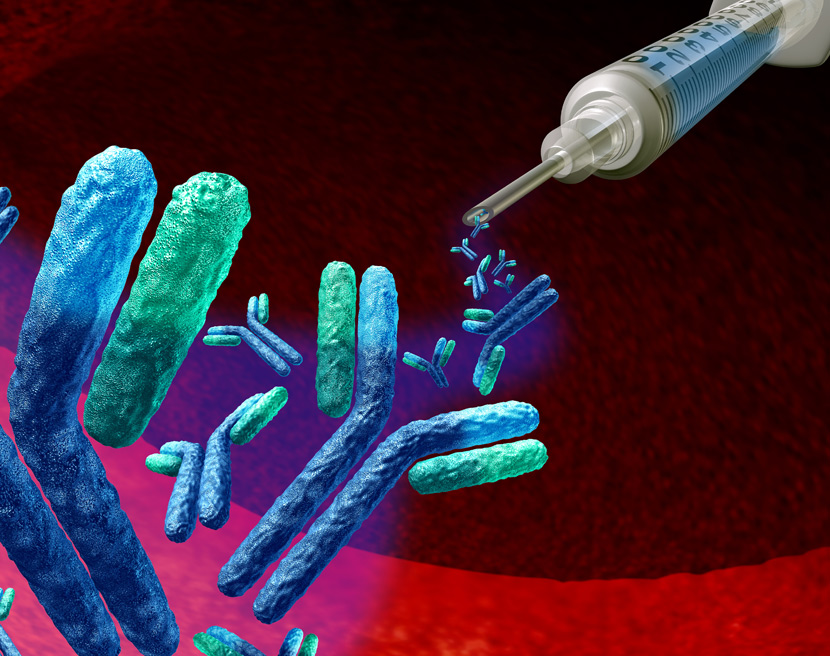
When an infectious pathogen (bacteria, virus, fungi, parasites) invades the body, the immune system produces antibodies (or proteins) to destroy the harmful organism.
Antibodies mistakenly attack the brain
In some people, the immune system goes awry and produces antibodies that mistakenly target portions of healthy cells in an area of the brain, known as the basal ganglia.
Targeting the
basal Ganglia
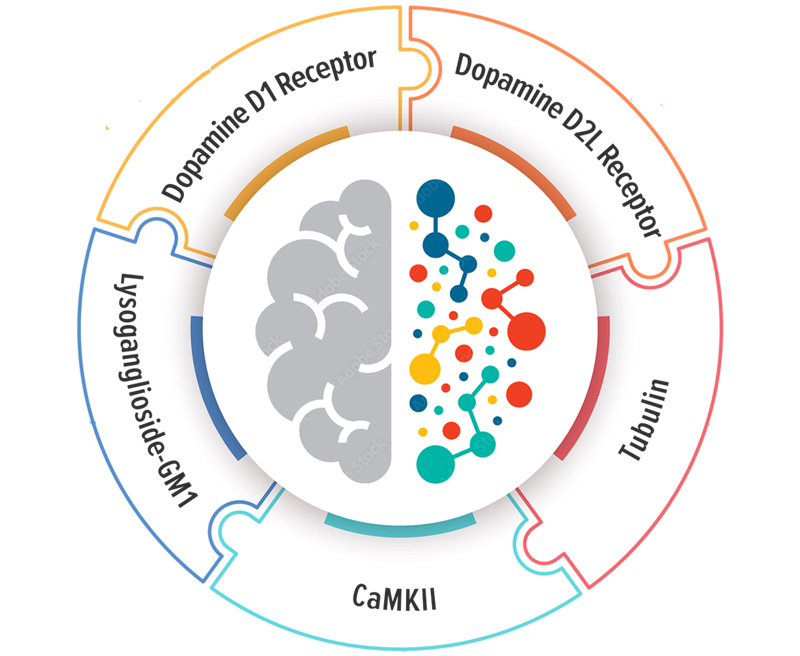
These “autoimmune antibodies” can bind to or block neuronal targets (Dopamine D1 and D2 receptors, Lysoganglioside GM-1, Tubulin) in the basal ganglia.
Disrupting how cells function
When autoimmune antibodies are directed against these targets in the brain, it can disrupt the normal function of cells and receptors.

Triggering Brain Inflammation
This autoimmune response can also lead to brain inflammation in the basal ganglia, a region of the brain responsible for movement, emotions and thoughts.

Resulting in Neuropsychiatric Symptoms
This, in turn, can lead to the onset of various neurologic, psychiatric and/or behavioral symptoms including OCD, mood disorders, eating disorders, tics and seizure-like episodes.
Could this be happening to you?
Find out if your neurologic or psychiatric symptoms may be due to an autoimmune response.
Could this be happening to you?
Find out if your neurologic or psychiatric symptoms may be due to an autoimmune response.
The Autoimmune Brain Panel™ is a high-complexity blood test that measures the levels of autoantibodies directed against specific targets in the brain associated with psychiatric and neurologic symptoms.
Elevated levels indicate that symptoms may be due to an underlying infection-triggered autoimmune dysfunction.
Proper treatment can reduce/resolve symptoms
Proper treatment can reduce/resolve symptoms
Identifying whether symptoms may be due to an autoimmune process is important, since therapy focuses on treating underlying infections and the immune system, rather than treating solely with psychotropic medications.
- Treatment typically involves eradicating the infection, reducing inflammation, and as necessary treating the immune system with immunomodulatory therapies.
- Early diagnosis and treatment has been shown to improve chances for a full recovery. 6
- With proper treatment, symptoms/behaviors often significantly improve or resolve completely. 7
Ordering The Auotimmune Brain Panel™
The Autoimmune Brain Panel™ can only be ordered by licensed healthcare providers authorized to order laboratory tests. The Panel can assist your provider in determining whether your neuropsychiatric symptoms may be due to an underlying infection-triggered autoimmune condition.
Requisition Form & Provider Information
Download and take this information to your provider to begin the ordering process. (Requisition for U.S. patients only)

Videos: Ordering & Understanding Test Results
Watch our FAQ videos covering the following topics: billing and insurance, shipping instructions and understanding test results.
How To
Order and Costs
The testing process begins with a licensed clinician submitting a requisition.
References
- Köhler-Forsberg O, Petersen L, Gasse C, et al. A Nationwide Study in Denmark of the Association Between Treated Infections and the Subsequent Risk of Treated Mental Disorders in Children and Adolescents. JAMA Psychiatry. 2019;76(3):271–279. doi:10.1001/jamapsychiatry.2018.3428 https://jamanetwork.com/journals/jamapsychiatry/fullarticle/2716981
- Benros ME, Waltoft BL, Nordentoft M, et al. Autoimmune Diseases and Severe Infections as Risk Factors for Mood Disorders: A Nationwide Study. JAMA Psychiatry. 2013;70(8):812–820. doi:10.1001/jamapsychiatry.2013.1111 https://jamanetwork.com/journals/jamapsychiatry/fullarticle/1696348
- Hollander, E. Interview: Developing Guidelines for Treatment-Resistant OCD. Medscape. https://www.medscape.org/viewarticle/507104
- Dubey D, Alqallaf A, Hays R, et al. Neurological Autoantibody Prevalence in Epilepsy of Unknown Etiology. JAMA Neurol. 2017;74(4):397–402. doi:10.1001/jamaneurol.2016.5429 https://jamanetwork.com/journals/jamaneurology/fullarticle/2599939
- Al-Harbi KS. Treatment-resistant depression: therapeutic trends, challenges, and future directions. Patient Prefer Adherence. 2012;6:369-88. doi: 10.2147/PPA.S29716. Epub 2012 May 1. PMID: 22654508; PMCID: PMC3363299.
- Shin Y-W, Lee S-T, Park K-I, et al. Treatment strategies for autoimmune encephalitis. Therapeutic Advances in Neurological Disorders. January 2018. doi:10.1177/1756285617722347. https://journals.sagepub.com/doi/pdf/10.1177/1756285617722347
- Brenton JN, Goodkin HP. Antibody-Mediated Autoimmune Encephalitis in Childhood. Pediatr Neurol. 2016 Jul;60:13-23. doi: 10.1016/j.pediatrneurol.2016.04.004. Epub 2016 Apr 12. PMID: 27343023. https://www.pedneur.com/article/S0887-8994(15)30139-9/pdf